Endo Battery
Welcome to Endo Battery, the podcast that's here to journey with you through Endometriosis and Adenomyosis.
In a world where silence often shrouds these challenging conditions, Endo Battery stands as a beacon of hope and a source of strength. We believe in the power of knowledge, personal stories, and expert insights to illuminate the path forward. Our mission? To walk with you, hand in hand, through the often daunting landscape of Endometriosis and Adenomyosis.
This podcast is like a warm hug for your ears, offering you a cozy space to connect, learn, and heal. Whether you're newly diagnosed, a seasoned warrior, or a curious supporter, Endo Battery is a resource for you. Here, you'll find a community that understands your struggles and a team dedicated to delivering good, accurate information you can trust.
What to expect from Endo Battery:
Personal Stories: We're all about real-life experiences – your stories, our stories – because we know that sometimes, the most profound insights come from personal journeys.
Leading Experts: Our podcast features interviews with top experts in the field. These are the individuals who light up the path with their knowledge, sharing their wisdom and expertise to empower you.
Comfort and Solace: We understand that Endometriosis can be draining – physically, emotionally, and mentally. Endo Battery is your safe space, offering comfort and solace to help you recharge and regain your strength.
Life-Charging Insights: When Endometriosis tries to drain your life, Endo Battery is here to help you recharge. We're the energy boost you've been looking for, delivering insights and strategies to help you live your best life despite the challenges.
Join us on this journey, and together, we'll light up the darkness that often surrounds Endometriosis and Adenomyosis. Your story, your strength, and your resilience are at the heart of Endo Battery. Tune in, listen, share, and lets charge forward together.
Endo Battery
Finding Strength in Suffering: Ellie’s Battle with Endometriosis As a Licensed Counselor
Send us a text with a question or thought on this episode ( We cannot replay from this link)
Have you ever felt dismissed or misunderstood when discussing your chronic pain? Ellie, an endowarrior and licensed professional counselor, addresses this important issue as she shares her personal journey with endometriosis. We hear her firsthand experiences dealing with chronic pain and periods, and her struggles to get a diagnosis in a medical community that often overlooks these conditions. Ellie's story will inspire you, and her insights will shed light on the complexities of living with endometriosis.
Imagine living with a complex web of chronic pain, endometriosis, and eating disorders, all while trying to maintain your mental health. Ellie invites us to explore this labyrinth with her as she discusses the difficulties of managing food sensitivities, engaging in meaningful conversation with our bodies, and maintaining mental health in the face of chronic illness. We delve into the world of body grief - the grieving process for the gap between the life we envisioned for ourselves and our current reality - and how to navigate this process with grace and understanding.
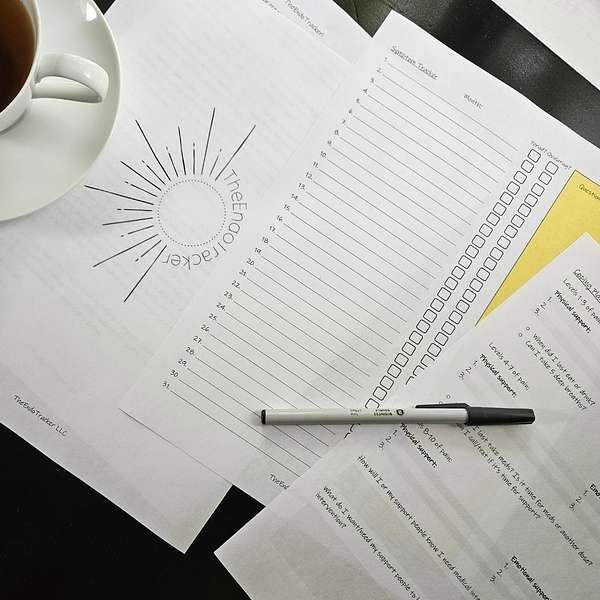
But it's not just about the struggle - it's also about finding solutions. Ellie introduces us to the EndoTracker, a tool she developed to help endowarriors identify cyclical patterns and manage stressful periods. With sections dedicated to documenting body grief, it becomes a trusted companion for those living with endometriosis. We also discuss the importance of self-advocacy and support systems in managing mental health while dealing with chronic illnesses. Listen in, and join us in this empowering conversation about living and thriving with endometriosis.
Endotracker on Amazon
etsy downloadable
Website endobattery.com
Welcome to Indobattery, where I share about my endometriosis and adenomyosis story and continue learning along the way. This podcast is not a substitute for professional medical advice or diagnosis, but a place to equip you with information and a sense of community, ensuring you never have to face this journey alone. Join me as I navigate the ups and downs and share stories of strength, resilience and hope. While navigating the world of endometriosis and adenomyosis, from personal experience to expert insights, I'm your host, elana, and this is Indobattery charging our lives when endometriosis drains us. Welcome back to Indobattery. Today, I am joined by my guest, ellie, and she has a perspective that is unique to her but will also allow you to feel seen in your journey with endometriosis. So go ahead and grab a cup of tea or a cup of coffee and join us as we unravel just her story and the things that she is doing to change the community for endometriosis. Here we go. Welcome, ellie. Thanks for coming on. Thanks for joining me. I was introduced to you by Pelvic4pt. Yes, I can say that.
Speaker 3:Yes, magical unicorn human.
Speaker 1:The magical unicorn human.
Speaker 1:But your story is one that I think a lot of people can resonate with. But you also have a unique perspective because you're not just not just I don't say that lightly you're not only an endowarrier, you're also a licensed professional counselor. So you see things from a different perspective, a different lens, not only as a patient, but you're seeing this also as a practitioner of sorts. But you have the ability to see life differently as well, and I love that. We've just been talking a lot. That's why I say this. So can you give us a little bit of a background about your story and who you are?
Speaker 3:Sure, sure. I'm one of the many who it took a long time to get diagnosed with endometriosis. My pain really started picking up at about 18, pretty noticeably, and I was just told this is how it is Periods are painful. We learn to cope, we learn to adapt. We treat people with kindness, regardless of what's happening, and over the years the pain just continued to get worse and I got more and more creative with different solutions to well, what if I use an ice pack? What if I use a hot pack? What if I tape hand warmers to the insides?
Speaker 3:of my jeans to get through these days where you know I can't call out its worker at school or both or. And did end up seeing a gynecologist in my early 20s and the response she was very kind, but it was very much take more ibuprofen or we can try birth control and go from there. I did not respond well to birth control and so I just started taking more ibuprofen and thought, well, this is just how it is and I just need to learn to work it through and maybe I'm just maybe I'm just like overly sensitive to pain and you know it'll be all right.
Speaker 3:Everybody hurts on their period.
Speaker 1:But there wasn't a diagnosis at that time. That was just going over your symptoms. It wasn't hey, you have endometriosis. It's hey, periods are painful. Go ahead and take this ibuprofen Exactly.
Speaker 3:Yeah, so that took me to only a couple of years ago. I'm in my 30s now and I don't remember exactly how I ended up. My sisters had started seeing a pelvic floor therapist and were like this is amazing and has been so helpful for all these places in my life. You really should go see her. And I was like, well, I don't have anything that she could help me with, because periods are painful guys. And I did end up caving and going to see her and she was like, hey friend, I really think we have more going on. Here's anyone ever talked to you about endometriosis, which I had Googled, like what is going on, you know, and that had I had seen it before online, that word but I think because I couldn't tick off every single symptom in the list, I was like, well, that can't be me.
Speaker 1:Isn't that funny how we think like we look at things on online, on the Google is some call it on the Google Dr Google the Dr Google and just because we don't see every symptom on there, we automatically say, oh, that's not. Yeah, that's not the case, we can't possibly have that.
Speaker 3:Yeah, my periods are very regular. I don't you know. You know and and I'm only in you know everybody's in pain on their period and I can still work. So I mean, I can work with a hot pad stuck to my insides and like the hand warmers taped in my pant lining and every time I walk into the office everybody's like oh, ellie, are you feeling okay today? And I'm like, yeah, I'm just on my period, it's fine.
Speaker 1:Did you announce that every time you walked into the office? Basically, that's awesome.
Speaker 3:Because people saw me and were like oh my God, you are not well and I'd be like oh, it's just a period, everyone feels not well. Yeah. And I did get sent home from work a couple of times because they were like you just look terrible, you're having a terrible time, you're like, and now.
Speaker 1:I'm having complexes because I look terrible now Like I feel terrible. And now you're telling me I look terrible. Thanks a lot for that.
Speaker 3:I know. So I have to use one of my days of PTO for this. So it took a little while. I kept telling my pelvic floor PT. I kept telling her like no, no, I don't think this is actually it. And then also, at the same time, being, well, I don't want it to be that. So, and what if? What? If? I'm like sure, let's do excision surgery, let's go in, and then it's not there. And then I finally come to terms with how, just how miserable I really am on a regular basis and that's not the answer. And now I've spent all this money and all this time and we're at square one, like we have no answers. And she just kept like coaching me through, like I really think that this is something that you should pursue and talk to an expert about.
Speaker 1:And she is a little pushy not pushy in like the bad way, but she will continue to advocate for you in that space of like I can't be the end, all be all with this, like you need to see someone that can really genuinely help you with this. I think we do need to mention that you are the sole provider for yourself, too, so there was a lot of concern there when you're talking about surgery and treatment and a really expensive disease. We all know that there's so much of this that isn't covered. You're you know we were just talking about the amount spent on feminine product or period products that are. You know it feels like a waste, but yet you have to have it, and so you're not only dealing with the financial part of that and you were in were you in school a lot of this time as well.
Speaker 3:I was in school and then part of the process to become a licensed professional counselor in Colorado is you have to do postgraduate supervised practice. So you're making very little money for until you get your 2000 hours supervised, which a lot of hours, a lot of hours.
Speaker 1:I mean, if good, like we want that right.
Speaker 3:You definitely want the oversight and the support you know in those first years and it's a long time it's a long time where things feel pretty. You know I don't have extra flex in the budget for things, so surgery or care, or you know, I didn't go to the doctor, I didn't, I just tried everything Google said, you know, to try and drink teas and I don't know, tried different, like lotions, like the warming balms, and you know, just to try to keep everything together so that I could keep working and yeah, I think that's what a lot of us do is, the expense of the disease is not one that a lot of us can really afford, and yet you can't afford not to do something about it.
Speaker 1:You get stuck in that conundrum of sorts because you're like okay, I need treatment or help, but I also need to make a living, and the living is not quite as much as the disease is costing me. So what do I do now? You know it's like do I take out a loan for this? Do I, you know, work extra hours, which I can hardly work now.
Speaker 3:So it just feel like that is a challenge. Working more hours brings up your stress, which makes your pain worse. You know, it's just. It's a very tricky position to be in.
Speaker 3:And so for a lot of years I just held myself together with whatever I could cobble together and, like I said, it wasn't until the last couple of years that I got connected with an excision specialist and did end up having excision surgery about a year and a half ago, which was definitely the right choice for me and because I'm my sole provider, it's me you know, that was very stressful to try to figure out how do I do this.
Speaker 3:And then again, what if they go in and there's nothing there, Right? So that was actually my first question coming and coming out of anesthesia. My doctor was standing at the end of my bed doing something in the chart and I said did you find it? And he said, are you awake right now? And I said yep, Did you find it? And he said yep, and that was a huge in that moment. It was a huge relief to be like, oh my gosh, we found it, we found it, we found it.
Speaker 3:I have an answer for at least part of what's happening. So and yeah, I know that I'm very aware that excision surgery and some of these treatment options insurance does not cover for a lot of folks. And I did end up making a job change a couple of years before surgery because I knew I was going to, I needed, I knew I needed more medical support. I just didn't know what that was and I knew that this job that I have currently the benefits would allow me to access care. So I think that too is an interesting part of anemitiosis. It's factoring even into where you work.
Speaker 1:Yeah, oh yeah, Because of things like benefits or capability, if you have a very physical job. Chances are if you're in the midst of a flare or your period is really bad. You may not be able to function if you're a nurse or if you're even a doctor, because you know it doesn't discriminate, I just think between here in the US and this is different for everyone everywhere.
Speaker 1:but here in the US, if you don't have good coverage, everything comes out of your pocket, which it sometimes it already does, because a lot of practitioners and doctors and specialists are out of pocket anyway. Your excision specialist was covered by insurance, which is huge, very fortunate, very fortunate. So that played a part in it, though, but I think that to say that it isn't still a financial strain because you're missing out on work at this point to even have surgery, even if you have coverage and benefits to cover those days.
Speaker 3:Using PTO. I think it was also hard to say hey, I'm going to be gone for this chunk of time, and that always feels a little risky you know, of I'm going to be out for weeks, and how does that impact how my job perceives me? Yeah, You're just only trying it. Yeah, the unseen costs.
Speaker 1:I think that if you live it, it's right there, but if you don't, harder to see and it's harder to explain that to even you know you're in the profession of like counseling and you're seeing all this stuff, but it's even still hard for people in your industry to see the major effects of endometriosis on a body, yes, and what it is capable of doing in our physical body, but in our mind and our fatigue? Did you have a lot of fatigue issues too? Oh my gosh, I did do so much.
Speaker 3:I always felt so bad but like the one to two o'clock hour. Yes, oh my gosh, it was like physically painful. You're so tired. Yeah, and nothing I did ever made it go away, it just ugh. And you're also trying to be present for people's stories and free and old sessions and providing your full and engaged self, and that's hard to do when you're in pain and so tired. Yeah, you know, managing your own symptoms, wanting to provide the best possible care.
Speaker 1:Right, it is hard, but something that we haven't mentioned yet is that you specialize in your counseling. What you typically do is disordered eating.
Speaker 3:Correct Yep Eating disorders.
Speaker 1:Yeah, yep, and so we were just talking about this before we started recording. But the correlation with endometriosis, if you have EDS, hypermobility or any kind of EDS or any sensitivities to food. It's very common for endometriosis patients to have some sort of eating disorder and it may not be your typical like we're not going to eat for days, your typical presentation. Yeah, the typical presentation of it. What does that look like when you're dealing with chronic pain, chronic illness, people with eating disorders?
Speaker 3:Yeah, so we do have a diagnosis. Avoidant restrictive food intake disorder would be what I would typically say. That would fall under Again, diagnoses are only there to help identify a set of symptoms and provide something that we can then attach treatment protocols to. In no way is it supposed to have any sort of moral implications which I think is always important to say when you talk about mental health diagnoses.
Speaker 1:Right.
Speaker 3:Just because we are still working through society, the stigma of a diagnosis Right. So with chronic pain, I do think that is the diagnosis I see most commonly ARFID, and I think it's a really tricky thing. Eating disorders in particular, it's the conversation between you and your body, the relationship between you and your body, and when your body doesn't feel safe to be in, when your body is constantly hurting, it's not going to feel nice to be in your body, and mindfulness exercises and a lot of those pretty common recommendations that you'll get from mental health providers are really hard. It's not a peaceful place to land in your body. Mm-hmm.
Speaker 3:When it hurts, when you're tired, when the signal's at sending you are agonizing. Mm-hmm. And that can become a pretty conflicted relationship. So I think too, when you start to build associations with when I eat this food, I feel bad or I experience these symptoms whether it's diarrhea or vomiting or stomach pain your brain is built to help protect you from pain, right, so it will reinforce those pathways, which then creates a whole new fun time of of like. I expect that I'll feel bad when I eat this.
Speaker 3:So I will, and then I feel even more like I will feel bad when I eat this. So I do feel, you know, it's a vicious cycle. Mm-hmm. And I think it's hard too, because when you're dealing with some of these diagnoses, there are food sensitivities and there are things where, yeah, there are some foods that your body may function better without. Mm-hmm.
Speaker 3:And then you're restricting foods and it just it can get really tricky. And so I think, having a lot of grace for yourself and a lot of you're not weird or wrong, or for I don't want to land in my body, I don't want to listen to what my body has to say, I just want to do what I want to do, Right? Or I'm too tired to eat? Yes, I'm too tired. It's too much effort, Like it all makes so much sense why we land where we do. Yeah, so you know, from a treatment perspective, how do we help re-engage in that conversation with our body of I don't like what you're telling me, right?
Speaker 3:now but we gotta live together, we gotta do this together, we gotta find a way forward, right? And what does that mean and what's doable? And I think for every person that's going to look a bit different. Yeah, which is always the fun, delightful answer. Yeah, and I think when you're dealing with complex things like EDS and endometriosis because folks experience variation of those things and then they overlay together, and then, yes, I think eating disorders are pretty common, or even just you know that disordered eating, difficult relationship with food, like there's a lot there.
Speaker 1:Right, and I think that what we have to be aware of, too, is that it's not your fault, no, and that is something that I feel like I don't know if you have heard this before but, it's just, I feel like when you go to a doctor sometimes and they don't really know or can really articulate, or they can't comprehend your pain, they don't know that you're not eating because you're in pain or you're too tired.
Speaker 3:They're like well something else is going on.
Speaker 1:Maybe this is what's really going on.
Speaker 3:They'll navigate you that direction.
Speaker 1:Or they say your pain, you're crazy, go see someone for it, Right. And then that I mean I'm the type of person that I say this because I know from my experience I will not eat if I feel like I'm crazy sometimes, because I can't organize the thought of, ok, I've got to take one step in front of the other, oh, now I have to go make myself food. What that's inconvenient, you know, and it's not that I'm trying to torture myself, it's that it's an afterthought, right? So when we're talking eating disorder and when we're talking pain management, and when we're talking.
Speaker 1:all of this, it's going to manifest very differently for everyone. Yes, and it's going to manifest, whether it's pain, whether it's because of mental health trauma, whether it's from just you know, it could just be that you're tired and you don't have the energy to get up and make something and nothing sounds good.
Speaker 1:That is often my issue of like. That doesn't sound good, why would I put that in my body? I have no appetite for that, you know. And to say that it's a disorder we need to destigmatize, that it is a way of managing how to fuel our bodies, I feel like. And connecting the mental state to the body state, and how do we combine the two?
Speaker 3:Yeah, I mean, I think anytime chronic pain is involved, it's just infinitely more nuanced and I think practitioners need to go to, about asking questions about OK, so tell me more about you know, when you didn't eat yesterday, tell me more about that, like what was happening for you. And then I think, on the other end, you know, trying to figure out a utilitarian eating is maybe what I would refer to it as which sometimes we do have to eat, even when we don't feel like. It Doesn't mean we can do that every time, you know. I mean I've had bad pain days where, no, I haven't eaten much because I have been in too much pain to get up to make something you know and then you're just doing what you can and that's OK.
Speaker 3:That's OK, you're doing what you can and also recognizing that you know for myself and my own symptoms. I know that my pain will be worse if I don't eat and I will have a harder time coping with that pain emotionally because my body does not have the fuel it needs for me to use my coping skills. So, finding things that even if it's rice cakes, I mean really simple things that I can keep on hand, that I don't have to cook, I don't have to heat up cans of soup, that's fine, that's great. They're shelf stable. You can use them when you eat.
Speaker 3:And so try to keep those always on hand, a few things that I know I can eat to try to give my body what it needs to go through what it's going through, regardless of whether I maybe feel like it or want to. So, striking that balance of like I can only do what I can do Right and also, again, for myself. I know I'll do better if I can even have a little bit.
Speaker 1:Right. Is there a correlation between eating and the heightened state of pain, mentally Like? Is there? If we're not fueling our body, does our brain signal to us that we're in a higher state of pain or distress? I mean you're?
Speaker 3:going to have a higher cortisol. You're going to have a harder time.
Speaker 3:You're like your body does, especially, I think of the fight or flight instinct rate of your body saying, hey, we're in a life-threatening situation, Like your body is doing a lot when you're in a lot of pain, when you're dealing with a lot of symptoms, and I think of it as I mean. You could use a lot of different metaphors. But if I had somebody out battling a forest fire, I wouldn't expect them to go without food and water and they are going to have a harder time making calm decisions. They're going to have a harder time knowing when they need to pull back, when they need to move forward. You're going to have a harder time. So, in general, if you're giving your body what it needs, your blood sugar is going to be more stable. Is my understanding? Again, I'm not a medical provider.
Speaker 3:But your blood sugar is going to be more stable, which is going to help you be more stable. Your emotions are going to be more stable. You're going to be less likely to go into that fight or freeze response, which pain is a trauma. Yeah, so that would not be uncommon for you to have that kind of a response. I don't have the specific research, but caring for your body as it does its best, it's always always giving you 100% of what it has Always, and that 100% may not be the 100% that we want, right, you know, it might be about 1% of what we feel like we should be able to do, but it's 100% for the day.
Speaker 3:It is always it's 100%.
Speaker 1:That means that we need to give ourselves a little bit more grace than we do, because we aren't going at the pace that society has told us that we need to go, and I think that is the other part of this that I feel like for me has been a challenge, because then I've dealt with more guilt.
Speaker 1:Associated with having a chronic disease is the fact that I have felt lazy, like I felt like I just need to sit here, and we always talk about give yourself grace, sit down, take a break, do what you need to do with your body, but that doesn't necessarily translate to my mental. Yeah, okay, my mental grace, if you will Like it doesn't translate to.
Speaker 1:It is okay to sit down, and there are moments that I am better than others, but it almost creates more of a trauma in my head sometimes when I don't sit down. Yes, and so it's a really good thing to remember that your body is giving you everything that it can. Yes, you know, that's why people say listen to your body. Well, if it can only give you what you think is 5%, it's giving you at 100, even if you think it's not.
Speaker 3:Yes, exactly, exactly.
Speaker 1:Ugh, where were you my whole life?
Speaker 3:I know I'm sorry and it's something that I tell myself. Like in the last month I have had to tell myself I have cried over like I want it. I want more than what my body can do for me right now. And this is it. This is what it can do, this is what my body can do, this is it's 100%. And if this was my friend, if this was my niece or my nephew or a child, I would be like, oh my gosh, you're doing so great, right so. And for me, then that pushes more into like, oh, I can give you compassion. Then I can give you empathy.
Speaker 3:I can say you are doing so great, while also honoring the fact that I'm frustrated and I want to be able to do more, and I want to be able to see more and be in less pain and be more. Quote unquote normal. Oh what is normal. What is normal we say? I think we say that, but then I think we all also have an idea in our heads of what it is.
Speaker 1:Yeah.
Speaker 3:And then we hold ourself to that standard of well, this is normal, and then we beat ourselves up for it, which is like we become our own collateral damage. Oh yeah, and that in this moment, with the margin I have, I can be like, oh, that's heartbreaking, that I can't honor that my body is doing, she's giving her all she's got. Yeah, you know, yeah. So I think the more that we can be aware of that, the more that we can start shifting those mental patterns to have more grace, to have more space, and then, weirdly, we're more able to cope with pain. I am more able to cope with pain when I can say, okay, this is what you can do, right, and this is what we've got. And okay, I see you doing your best. Okay, I hear you. Right, I will be here with you and we will figure the rest out.
Speaker 1:Yeah, yeah, but that also doesn't mean that you can't grieve what you wish you could do.
Speaker 3:Oh yeah.
Speaker 1:I hear so many people say I feel like I'm grieving right now and you do. Oh yeah, All the time, oh yeah. What are some of the stages of grief? I know that some people are aware of that and some aren't, but what are some stages of grief when you're dealing with chronic pain and a chronic disease?
Speaker 3:So this is a newer area for me, but there is a terminology I don't remember her name, jane Mattingly maybe is one who talks a lot about and she has a book coming out early next year. She talks a lot about body grief and chronic pain and how this is what I thought my life would be and this is what my life is.
Speaker 3:And you have to grieve, really grieve, the distance between the two of those things, and so the stages of grief are more of a what this one person noticed about grief and put together, versus something that we've put together through a research study or something like that. So I'm definitely curious to hear more about it, but it's not a new concept. I guess the idea of body grief and how do I be in a body that feels so different from everyone else and on a daily, minute by minute, sometimes reminder of like I can't do that, I can't do that, I can't do that, I can't do that?
Speaker 3:I can't do that that's, especially in Western culture, really hard to honor because we just struggle in general with honoring grief.
Speaker 3:So then, when you add in chronic pain and unseen conditions where people are already questioning, well, you're not in that much pain. Everybody has a period that hurts you're dealing with a lot of complexity. That's very hard to tease out If you've never heard the word body grief or endometrosis or those are very real things that are super important and healthy and a part of the process, and you can't not do it, you can't skip it. Grief is always something that you have to sit with until it says otherwise.
Speaker 1:And I know just from personal experience in I've lost my brother at a really young age he was 15 when he passed away and I remember my mom, her stage of grief she didn't wanna eat and I think the same can be true with body grief and not wanting to eat and not wanting to treat your body kindly because it's not being very kind to you, and I think I mean again, I'm not the licensed one here, but just personal experience would lead to say that if you are grieving on top of everything else that you're feeling, if you're having body grief or you're grieving in some way or another, you're less likely to want to eat. Or you could overeat sometimes. And then you feel worse because your hormones are all out of whack right.
Speaker 1:So when we're talking about all of these things, they're very complex and it's a very hard thing to navigate and you do need to talk to someone who is licensed. It is not just your mental state, especially when you're dealing with a chronic illness like your body and your mind are they work together or they don't? Sometimes yeah.
Speaker 1:Yes, right, yes, yes, and so just trying to navigate. Okay, am I being kind to my mind, am I? Being kind to my body. Am I honoring my grief, Mm-hmm absolutely 100% Like it's gonna look different for everyone. Yeah. But they can all go together hand in hand. I feel like just from my experience of okay, I'm grieving, now I don't feel like eating, but how can I get broth in me Perfect, you know, and simple things like that how can I just get some broth Just to put something in my body?
Speaker 3:Because if we had a dear friend who was grieving the loss of someone close to them, extremely common and in fact is not considered I don't love this word, but it's not considered pathological for someone grieving to not eat up to a certain point.
Speaker 2:And then we start looking at okay, is there more happening here?
Speaker 3:And if that's considered normal and does not meet criteria for any diagnosis, like there is some grace here for, yeah, if you can, if you know, we would show up to our friend's house and we would offer them what we could. Right.
Speaker 3:You know, maybe that is broth Right. We would show up and say, hey, yeah, you had some broth, great, right, let's start there. And when you're ready, you know, they'll get back into it. But when we're in that intense period of grief which absolutely can happen coming to terms with a diagnosis like endometriosis, if or just my life isn't gonna look like I thought that it was going to, you know, I think there's so many things that come with endometriosis whether that's infertility difficulties, and you know they're painful, painful things that come from this as an extension, regardless of the original endometriosis diagnosis like grief, I would be more concerned as a therapist if someone were not grieving. I would have more concern for that and as a part of that grieving process, yeah, that is also gonna impact your appetite, your sleep, your mood, all of those things. And if that persists and you know you're really having trouble coming out of that, then yes, we definitely need to involve someone to help support you, support your body, support your mind, support your emotions, and grief is gonna it's a systemic impact.
Speaker 1:Yeah, this disease is a whole body, whole life, whole everything. Yeah, it's what a delight, yeah, isn't it though? Isn't it though? And have you walked through that yourself in your diagnosis? Because your diagnosis, this is not like you've had it for years and years and years.
Speaker 3:This is really kind of fairly new yeah, the diagnosis itself yeah, it's only been a year and a half that was confirmed. So, yeah, definitely. I mean, like I said, in the last month I have cried out of frustration because I was asking my body to do what I thought was reasonable and normal and watching my friends and my family having no issues and being like I don't understand. I don't just have periods I have to plan for, I have to bring things.
Speaker 3:I have to it's a more complicated event and I do feel sometimes very resentful of that, of this is not what I would have wanted to be spending my time on. So trying to honor that and that those feelings are real and valid and a part of the process, they're normal, they're healthy and I don't want to live in a place of resentment. I can camp out there for a while, that's fine, Appreciate the view, but I don't wanna build my house there. I don't wanna live there because I have too much at this point in my relationship with my body.
Speaker 3:I have too much respect for it my body and myself to live there and she's done too much. Yeah, she survived too much, and that is a daily practice. That is a when I'm feeling more grouchy, that's a lot harder to say. So I you know. I wanna couch that I have too much respect for my body in. We're human and that's gonna fluctuate. That's not a static state. That's gonna fluctuate and that is also okay. So I think for folks to understand that you're not just gonna like arrive at some in years of that magical state, or in the mullies.
Speaker 3:Yeah, and the more you, the more that I learn about my symptoms and the more that I learn and the more that I integrate, like, oh, that's what that was when I told that provider, like it was the weirdest thing that my vision, my periphery, it went kind of gray and I don't know what that was.
Speaker 3:Yeah, and this is so weird. It's so weird that that happened to me and not having the provider say so. Hon, you almost passed out because you were in so much pain. Nobody ever said that to me. Nobody ever told me and I don't know what I thought was happening, but I didn't think it was that I was about to pass out. Yeah, and nobody told me. Yeah, and I think I feel that's one of the pieces I think I've been trying to integrate of like I didn't understand what my body was telling me and I went to people to help me understand what was happening and they didn't have any tools for me and I. That is the part right now that I think I struggle the most, with anger and hurt and grief around of like that was seven years ago when I told you that yeah.
Speaker 1:I could have solved this a long time ago.
Speaker 3:It was seven years ago. You could have been like hey, Ellie, that's weird, that's weird yeah.
Speaker 1:Which and that's a good segue to what you're doing now and the things that you have created because that piece of it of tracking things, being able to tell your doctor okay, I am feeling this way, when this happens, my body is doing this. You created a tracker, an endometriosis. Is it endometriosis specific or just a symptom tracker? So tell us kind of what you've created with that to be able to help navigate talking to providers, family members and everyone in between.
Speaker 3:Yeah, so I did create a symptom tracker. It is geared specifically towards endometriosis, but I think a lot of folks could potentially use it, because my lived experience is endometriosis. Mm-hmm.
Speaker 3:That's a lot of what I drew from, but basically I wanted to create a accessible, affordable tool for folks to be able to, a month at a time, write out what's happening for them with regard to their symptoms, to also be able to identify. This is when I was on my period, this is when I was ovulating, because there's so much cyclical symptoms with endometriosis, and my hope being that then you could lay out a couple months at a time and really see what your pattern is with a provider, with a family member, because my experience was I'd come in and say things like, yeah, I'm losing peripheral vision, it isn't that weird, but they always felt like standoff events to me. They didn't feel like, no, no, this has happened several times to you on your period. So, like I said, I wanted to create something that is affordable, that is easy to use, that you can see at a glance what's happening, and so it's called the endotracker All one word, so no spaces.
Speaker 3:It's on Amazon as a printed booklet, and then I also have a printable version on Etsy. So that's the first resource that I created, because when I was trying to track, when the pelvic floor PT was like hey, I think you need to look into this. One of the things she recommended was tracking my symptoms to be able to show the doctor this is what's happening on a month to month basis and I just didn't find anything. It was all so complicated and so many things to click through and if you had an app and it was just so overwhelming and when you're already dealing with fatigue and pain and all this other stuff, it's like I need something that's simple, that I can lay by the side of my bed, that I can roll over at the end of the day and be like, yeah, my pain was a six, my GI system, I had these symptoms and ta-da Right you know, this is how I was feeling today.
Speaker 3:Right.
Speaker 1:I was at a heightened state of stress.
Speaker 3:Hystress.
Speaker 1:I was having a hard time with my body like able to really write down what you were feeling, how you were thinking. What is your symptoms? Am I on my period? Am I not? That type of thing is kind of what you were like okay, let's do this.
Speaker 1:I'm a pen and paper kind of person. I am not tech savvy enough to open apps. In fact, I have a ton of apps that I had used, but I would use it for like a day or two and that was kind of it. This is such a tangible way that anyone could get a hold of it and you've made it so affordable I mean less than $10 to download and continue printing off, if you want?
Speaker 3:Yep, there's a monthly version and there's a yearly version. So if you just wanted to get the monthly and print off three and just do it for three months, great. If you want to get the yearly one and start wherever month you're in and see what your body's doing for a year, great. I also included in there, for that particular resource, coping plan so that when you're having a hard time, you've got a tangible, you've got a physical reminder of like, okay, how are you taking care of yourself, not just physically, but mentally. How are you taking care of yourself? Because it takes a lot of mental fortitude to experience that much pain. So how are you caring for yourself, mentally, emotionally?
Speaker 3:So that is also included in the Endo Tracker as, at different levels of pain, what are you doing? So that, also, if you have your support person, your loved ones, you wake up, because I've had this happen to me wake up in the middle of the night and you're like in an eight or a nine and I have had to call people using Google, being asking Google to call a family member for me to come and help because I could not care for myself. I was in so much pain, but I also don't have the ability to tell them what it is that I need, necessarily so to be able to have something that your family members or loved ones, your support people, they know this is where you go. This is what I can tell you. A number I can tell you where I am right now on a pain scale.
Speaker 1:And this is what I need to be able to bring me back down Without having to say it. They can look, it's like their guideline to help them. Help you, yes and not just physically, but emotionally.
Speaker 3:This is what I need. I mean, I've had grocery store clerks be like what do you need? What is happening? You are not well.
Speaker 1:Do we need to call someone for you?
Speaker 3:And that was very humbling. But yeah, so this is created partially with that in mind, of this is how you can help me. This is what I need.
Speaker 1:It's also something tangible to hand to your doctor, yes, which I think is huge, because we don't always put the pieces together and it may not be something that we think is a big deal in how we translate our care or how we translate our pain to, or even what we do to help our pain. So, say, we have heating pads. That's the only thing that's going to help you. Or hand warmers stuck to our pants so that we can get mine.
Speaker 1:We may not think much of that, because it's we've always been so normal, so normal right, but a practitioner or a care provider might look at that and say that's not really that normal.
Speaker 3:Yes, yes, help you. You are encapsulating your experience and the provider can look at it and be like this is outside of the normal limits. This is again I don't love this word, but this is pathology. There is a diagnosis here. And we can treat this. That's significant, yeah, yeah, because we're a frog in boiling water and don't realize that we're quite as miserable as we are. I think we know we're miserable, but I think you don't know how much space it really has taken up until you have someone point out, right?
Speaker 1:So Well, and also, I think too, if there's a space to write down what a care provider has said to you that maybe was triggering and that was something that you could take to a mental health provider and say this was triggering to me and this is why that was triggering to me. Or even when you're seeking care through another provider and another doctor and saying this doctor, this is what they said to me, it triggered this emotion, this response within my body. And is there a way? Is this can't be normal, Right, Like, how can we A avoid this happening again, Right, but also, B, how can we work through this so that my body doesn't have that response? Or is this responding a certain way? And I don't know the answer to that all the time, but I do think that there is a correlation. You know, we can maybe correlate how our body is responding on our periods or even post hysterectomy in my case, but what?
Speaker 1:my body is responding to stress. If, for instance, I had a care provider tell me that what I was going through was nothing, or that it was in my head, chances are my body is going to respond to that as well, and then I'm going to need help climbing out of that hole a little bit Right, telling our family members, telling our providers hey, I need help here.
Speaker 3:Right, I mean there is a section. That's a great idea. There is a section for questions for my providers which is on the side of the monthly specifically, so you can, in the moment when it's happening jot it down and have it ready to go, because I think I did feel badly about asking some questions and so I wouldn't. But if I had, in the moment, been like, hey, my body's having a really strong reaction to this and I'm documenting my symptoms, I'll just write it over here. You can't unwrite it.
Speaker 1:I'm sure you could scribble it out. Why is it scribbled out over here, exactly, exactly, momentary lapse of judgment, I don't know.
Speaker 3:I answered it for myself, no, but yes, because I wanted to have a place where, in those moments, ask the questions, like get the information give the feedback, and I know so many of us have had, if not bad experiences, just unhelpful ones, and I think not always because the providers I mean, they're stressed, they're tired, but I think a lot of times they just don't know. And so I think, yes, I did put a spot for questions for providers right on that form so that it can be a conversation. My hope is that it's a conversation and maybe they get to learn along the way too, with you.
Speaker 3:I have learned so much from my patients, my clients, over the years that DSM, our Diagnostic and Statistical Manual. It just can't encapsulate what it is to live with an eating disorder. In the same way that a doctor may be familiar with endometriosis, they may even be familiar with ways to treat it. We get to teach them what it is to live with it. That's so, so.
Speaker 1:We need to do more apparently. Yeah, but that's so good, and because now you're not in the diagnosis stage, you went into the surgery stage. And so you created a tool for people to help with surgery as well.
Speaker 3:Yes, so there's a surgery kit, which again was based off of a lot of my own experience preparing for surgery and feeling pretty overwhelmed and there's a lot of resources out there, but they all felt pretty disconnected to me and I want a to-do list and I want, here's, some things you should think about. So I put together this kit to go through. What are your meals going to look like? What is your comfort items?
Speaker 3:Because we all need comfort items when we're going through something hard and having a plan for that ahead of time. What are the to-dos of things that you need to get done before surgery? And then the back section of the surgery preparation kit is something to be used immediately after surgery. So every hour of the day has a line to indicate did you go to the toilet? Did you have food or water?
Speaker 3:Did you know what medications were taken so that anybody could come and assist with your care post-surgery and know what's happening? Yes, so that if it is just you, you know what you did when you have a place to write it down and be like oh yeah, I took that medication at 7. And I went to the toilet and it's something that you can take to your providers if you're having complications and they can have a really quick encapsulation of what your days have been looking like. And hopefully my hope is that that will provide I don't know just a general aid in what's going on, what's happening, because they know what your day is looking like, because post-surgery, I didn't know what hour, I didn't know what was happening.
Speaker 3:I was just trying to sleep and not move.
Speaker 1:You were just trying to survive.
Speaker 3:And then, yeah, yeah, I had a very sweet family member keep bringing me barbecue chips, because that was the only thing, but it was so fun. But do you even write that down?
Speaker 1:That was the only thing. Yes, barbecue chips, yes. Settle well with her. Yes. Just to get food in her. This is what she would like. Yes, so when they do a rotation or when you're going to your doctor, these are some of the things. And you know, I'm sure there is a correlation between the minerals and, like the, I know right. Everything in there, I don't know, I'm not going to get into that I agree with that theory. I agree with that it's usually what your body needs or what it can receive better and yeah, and, but just to fuel again.
Speaker 1:fuel your body when you don't want to write and your body can accept this Right and then but it's passing on that information between people and care providers and people caring for you, your support people.
Speaker 1:Yep, I wish I would have had this post-surgery so bad. I'm really. I'm like why were you not there with me? Sorry, I know, I feel like this has been a good session for me. Where's your bin mo? I'm going to need to bin mo here for this session, but I do think that it's so important to have these tools in place and you have made them so affordable.
Speaker 1:Yeah, and they are typically between Five and eight, five and eight US dollars, yes, and then, because you're kind and generous and this isn't like necessarily, you know you're not aiming to gouge anyone this is really truly a support piece. If you go onto the Etsy site and you put the coupon code Indo battery in there, you'll get 10% off, correct?
Speaker 3:Of the downloadable which is come on.
Speaker 1:That is like less than a cup of coffee. Yeah, for most people.
Speaker 1:And so this is a way and a tool that you can use that will help you in your journey trying to figure out the best care. But understanding yourself, I feel like that's huge. There's so much that I forgot about my journey to where I am now that I wish I would have had that peace, because I didn't have any of that and it was when I would go to the doctor. I'd have to remember what was that question I wanted to ask again.
Speaker 3:And what was I?
Speaker 1:feeling here and it was funny because, like my husband, would be the one, you often feel this way when you drink red wine. Yeah, you love your red wine but, you don't feel good when you drink it, that's real.
Speaker 1:That's so real. You had this response when you ate this type of food, or your period never stopped for three months. Yeah, yeah, let's track that. What did you feel in certain spikes in certain parts of the month? This is such a great tool that no one has to log in for, and I'm not saying that those apps are bad, I think if they benefit you and they work well for you great.
Speaker 1:Sometimes they're not financially accessible for some people. This is accessible for most people and you understand that. Being a sole provider for your household, you understand the financial piece of that. That's why you've made it the way you have. You also understand that you have multiple people coming into your circle trying to help you. Yes, I'm like when you showed this to me, I was like come on, why, why did I not have this? I was just glad.
Speaker 3:Yeah, I mean I'm not glad that you didn't have it to be clear. I think it's something that I wish I would have had as well, frankly, yeah, I looked for it and I just didn't find something that didn't feel way too complex or that it didn't fit my needs. So I hope and always open to feedback, but I hope that it is an aid for people and it just helps them figure out what they need and helps them have that conversation with their providers in a way that gets them care faster than.
Speaker 3:I got, and faster than many of us get, yeah.
Speaker 1:I think it's also good post-historectomy too, though, especially if you are for hormonal changes. Yes, Because I know for some people that have had a hysterectomy but maybe still have ovaries, they're still having some cyclical things that are happening, their imbalances. I think this is a great tool because it's not so set in stone. You can write out a lot of what's going on. It's not just endo specific, it is symptom tracker.
Speaker 3:Yes, symptom tracker with a specific gear towards all on one page and to identify where you're at in your cycle. So, yes, if you do still have your ovaries, is it this one particular? The 15th is this keeps the symptom, keeps cropping up, or whatever.
Speaker 1:Yeah, and we're going to talk about some other things off air that I'm going to give you and put on your plate, because I have ideas. I love it. Yeah, not just for endo. But I'm just saying I'm a hormonal mess half the time.
Speaker 3:I'm just women's health care is a ride, isn't it, though? So I think anything that we can do to help folks get care in a helpful way, I am all for, because it can be rough out there. So yeah, yeah, it absolutely can. I'm here for it.
Speaker 1:You also are using this as a tool to help family members that are in need as well. And so that is the other part of this is those little bits are just helping a family member going through a rough time. Yes, yeah, and I do want to be transparent in that this is not just a tool for you, but a tool to help your family.
Speaker 3:Yes, have a family member who has had some very serious health stuff that at this point looks like it has resolved, which is wonderful, and the health care system is very expensive. So, yeah, part of the driving force behind this was to create an ability to say, hey, I can help out with whatever groceries this week, I can cover that, I can cover the cost for gas in your cars. So, yes, yeah, this is a tool, this is a rounded tool. It's what I'm trying to get at.
Speaker 1:It's like this is not just something where you're like, oh, I just need to make a little lecture so I can get a pedicure. This month oh no.
Speaker 1:No, the driving force behind this was really not only to help those with endometriosis or any chronic or tracking need. It is also the driving force to really publish it and get it out. There was a way to help someone else in need, and so you downloading this tool, anyone downloading this tool, whether it be the Indotracker or whether it be the surgery toolkit is also helping a family member who needs the support as well.
Speaker 1:So I want to just say that this is not all for not. This is a tool. I'm just telling you. I firmly believe that you will get. Anyone can get use out of this. And it would be beneficial for anyone, but especially the surgery tracker, which isn't quite on Amazon. It's getting there and Amazon comes printed, so it's a little bit more expensive because it's printed for you for the year, correct?
Speaker 3:Yes, that one is just the yearly and it is more expensive to cover the printing costs. Yeah Right.
Speaker 1:And that one is right now just the Indotracker, but you're getting the surgery on there.
Speaker 3:But the Etsy is the surgery toolkit and the Indotracker, yeah, and those are 5 to 8 on Etsy and then the Amazon will be 20 for the Indotracker which is live and there now, and then I'm hoping to have the surgery kit on Amazon as a printed option before the end of the year. Yeah.
Speaker 1:So keep an eye out for that, and I will put a link in my bio for a way to get that as well. So if you're looking for that, I'm going to have a resource page for that. But I just want to say I would not have you on talking about this if I didn't find it beneficial for everyone and a tool for so many people who are struggling to put the pieces together, but also financially. Yeah, you really can't beat this, and I'm not just this is not a sales pitch, I'm just saying I really believe in it. So again, indobattery for the Etsy shop Yep, put it in there, you can get a discount.
Speaker 3:But if I can figure out something for Amazon, yeah, we'll figure.
Speaker 1:I'll keep you posted. Keep me posted. Yeah, yeah, linkin me that. But thank you for spending the time with me and I just feel like gosh, I just really feel like I need to Venmo you for everything that you've just given me in life. I appreciate that.
Speaker 3:It's very sweet. It's been lovely.
Speaker 1:Yeah, it's been so good. And I think that if you're struggling with anything that we've talked about, or even if you're just struggling trying to put the pieces together between your body and coping with that, with your mental capacity and state and you're just struggling, reach out to someone. There's people out there there is the crisis health line, but then there's also people that can listen and you're not alone. This is not your fault. This is a disease that is out of your control. Yep, in the way it responds to your body, yeah, but if there's tools that can help you manage it, then that's where we need to focus that energy. So thank you for bringing Link to that and just being a light in yourself. I just really enjoy you so much.
Speaker 1:Thank you. I'm so glad that Lee put us together, because it's been so fun just to get to know you and get to experience this and learn from you. So thank you so much. Thank you, yeah. Until next time, everyone, continue to advocate for yourself and for those that you love.